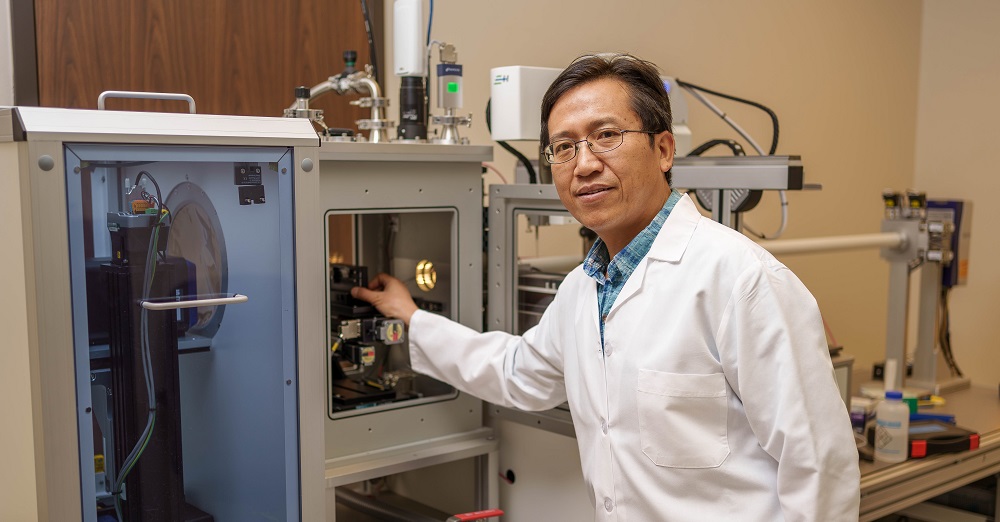
Hongjun (Henry) Liang, Ph.D.
For Texas Tech University System students and faculty who have an entrepreneurial itch, the Innovation Hub located near the Texas Tech University Health Sciences Center (TTUHSC) campus in Lubbock offers ongoing opportunities whereby faculty form teams eager to learn how to take an innovation from the bench to the marketplace. These opportunities are available thanks to the National Science Foundation (NSF) Innovation Corps (I-Corps™) program.
Teams participating in the NSF I-Corps™ program receive comprehensive training designed to take them from innovation to impactful development that goes beyond the laboratory. I-Corps™ teams may be formed for the regional and national levels, though teams wishing to participate nationally must be recommended by a regional I-Corps™ program such as the one available at the TTU System’s Innovation Hub.
Once a team reaches the national I-Corps™ program, they are required to conduct a minimum of 100 interviews over a seven-week period. During this process, known as customer discovery, teams complete their business model canvas by learning about potential customer pains, gains and value propositions. The process validates customers’ needs so that teams don’t spend time and resources developing something nobody wants, and it de-risks the innovation for future investors or industry partners. This summer, two teams from TTUHSC advanced from regional I-Corps™ programs to the national I-Corps™ program.

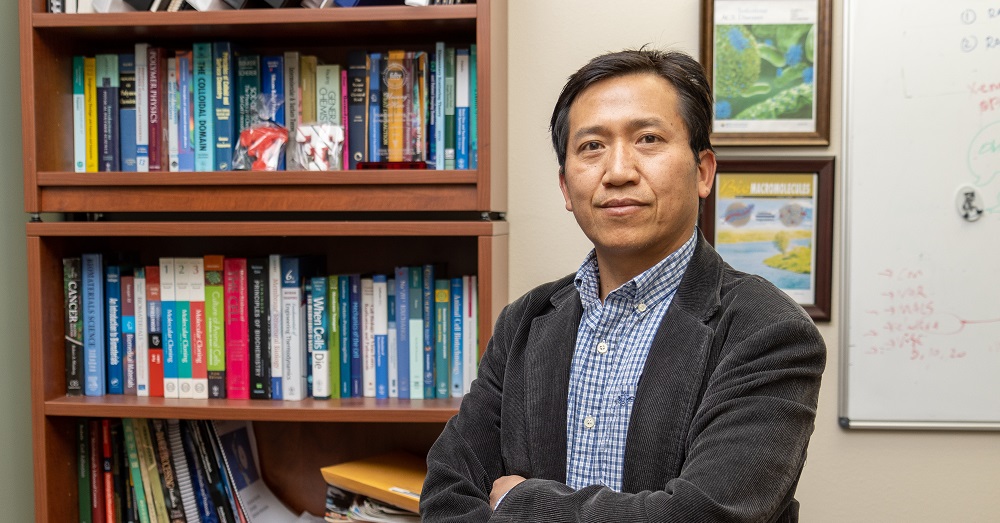
Alan Pang, M.D.
One team, led by Hongjun (Henry) Liang, Ph.D., a professor in the Department of Cell Physiology and Molecular Biophysics at the TTUHSC School of Medicine, is working to address antibiotic resistance using patented nanoparticles known as nanoantibiotics. Other members of Liang’s I-Corps™ team include Entrepreneur Lead (EL) George Hana, a doctorate student in the Department of Chemical Engineering at Texas Tech University, and Industry Mentor (IM) Angelina (Lena) M. Zappia, an Office of Research program director working in the Division of Research Innovation, Collaboration and Entrepreneurship (RICE) at TTUHSC.
The second team, led by assistant professor of surgery Alan Pang, M.D., is developing an algorithm-based system that will produce better treatment outcomes for burn victims. Pang’s I-Corps™ team includes EL Yifan Li, a TTU graduate student who is researching machine learning, image processing and computer vision; Technical Lead Jaewon Seong, a TTU graduate student researching machine learning; and IM Neal Weinstein, whose experience spans four decades in various industries with companies that have developed, manufactured and sold new products in international markets.
Big Things May Come in Nano-Packages
The Centers for Disease Control and Prevention estimates more than 2.8 million Americans contract antibiotic-resistant bacterial infections each year, with approximately 35,000 of those infections being fatal. To help improve those outcomes, the Liang lab is developing novel hydrophilic nanoparticles known as nanoantibiotics that target bacterial infections, especially those that are resistant to treatment with known antibiotics.
Hongjun (Henry) Liang, Ph.D.
The nanoantibiotics created by the Liang team resemble tiny hairy particles composed of many hydrophilic polymer brushes grafted onto synthetic or natural nanoparticles of defined sizes and shapes. These synthetic compounds are designed to kill bacteria via membrane disruptions using a different mode of membrane remodeling that damages bacterial membranes while leaving mammalian cells intact.
To date, Liang’s research has resulted in several peer-reviewed publications. He also was issued U.S. Patent #11,395,804 (“Hydrophilic Nanostructured Membrane Active Antimicrobials With High Activity, Selectivity And Biodegradability”) on July 26, 2022. He is optimistic that participating in the national I-Corps™ program will help his team take an important step toward moving their innovation from the lab to the marketplace.
“The I-Corps™ program is designed to train us to be entrepreneurs because we are from academia,” Liang said. “The primary aim of this program is not to support continued research discovery of your project; rather, it trains you to go out of the building, to get out of your comfort zone and meet people. Their lectures are about how you go from a bench-top product to a commercial product, how you're going to find collaborators and how you're going to find channels of distribution. It's designed to help us, as academics, gain some understanding about how commercialization works.”
The Liang team is continuing to conduct interviews and pitch their product to prospective customer segments such as marketing and business directors of pharmaceutical distributors that supply drugs to pharmacies, and administrators and marketing managers in hospitals, clinics, dental offices and other health care facilities that frequently purchase antibiotics. The goal is to identify a minimum viable product that will meet marketplace demands and remain financially feasible.
“Although we think we have an excellent antibiotic product to offer, in order to succeed you need to find the pitch and the right match to design your startup in a way that you're able to generate revenue and grow,” Liang said. “That's what they taught us and what we're trying to find out. We're trying to finalize our minimum viable product so we can start with a good business model.”
At the same time, Liang is not resting on the technology he and his team have developed. They have applied for an R01 grant from the National Institutes of Health (NIH) that has been favorably reviewed and revised for further consideration. If funded, the grant will help Liang continue to develop and refine his nanoantibiotic technology.
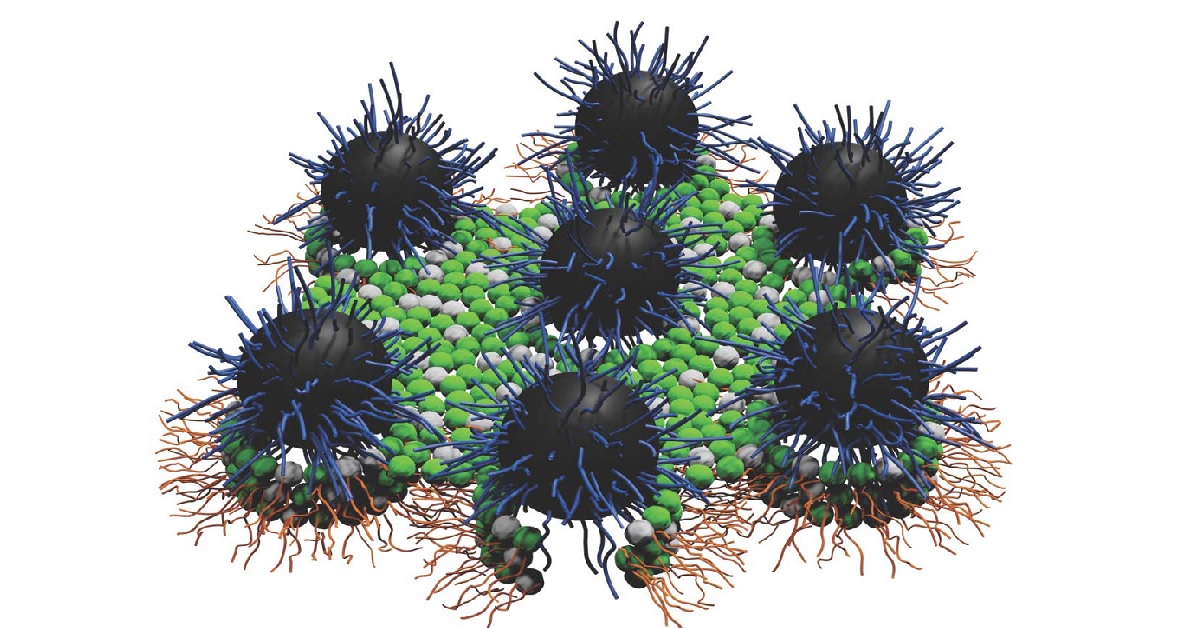
CGI of nanoantibiotics
“If you look at the pipeline for any antibiotic, it's a long game,” Liang emphasized. “It's not like you come out with something and from there, you're going to market it for clinical uses; it’s much more complex than that.”
For the Liang team, the long game will include conducting animal model studies and, once that is successful, potentially collaborating with the TTUHSC Clinical Research Institute to conduct clinical trials. Liang said those are important roadblocks to overcome before his innovation is deemed safe and effective and can enter the stringent and heavily regulated market for antibiotics.
“We still have other things to fix, but at the same time we think we're already in a very good position for a market pathway compared to a lot of other studies along this line,” Liang said. “We have the proof-of-concept for the new antibiotic design that's now protected by intellectual property, so we are in the very good position to exploit this new field. I think we are fortunate to have a local I-Corps™ program at the Innovation Hub. They are tremendous in terms of helping us to begin to form a start-up. I hope more people can take advantage of their training program.”
Machine-Learning Algorithm for Better Burn Outcomes
Burn injuries are responsible for approximately 400,000 hospital visits each year in the U.S. and are a significant cause of morbidity and mortality. Current diagnostics of burn injuries rely upon the eye of the beholder to use estimation charts such as Lund-Browder diagrams, which are based on a standardized diagram of the human body, to piece together a patient’s total burn surface area (TBSA).
The deeper the burn penetrates the skin, the worse the burn shock for the patient, so the TBSA measurement is crucial in defining a patient’s resuscitation for the first 24 hours of burn shock. Yet, Pang said, even the most experienced burn surgeons are accurate just 65 to 80 percent of the time in measuring indeterminate burn depths. The struggle with estimating TBSA is that inexperienced providers such as EMTs, non-burn physicians and nurses are not well versed in this type of estimating. This can lead to inaccurate resuscitation and misallocation of transportation resources, especially in West Texas, given its rural nature and 220,000-square-mile coverage area, which is approximately the size of France.

Alan Pang, M.D.
To help improve the TBSA accuracy rate, Pang’s team is developing a convolutional neural network that includes a machine-learning algorithm.
“Our method employs image processing and concomitant machine learning to measure TBSA and determine second- and third-degree burn areas, which can affect the amount of resuscitation,” Pang said. “By training this machine-learning algorithm, we could more accurately determine whether an indeterminate-degree burn will convert to a second- or third-degree burn, hence minimizing unnecessary or delayed surgery.”
Generally speaking, whenever someone gets burned, they are taken to a physician who may or may not specialize in burns. The physician can use one of several accepted tools to estimate a patient’s TBSA (e.g., the rule of nines or the Palmer method), which is crucial because the bigger the burn, the more of a systemic inflammatory reaction the body will have. And the bigger the burn and the reaction, the more fluids the patient will require during the first 24 hours when the body basically goes into shock.
“The body releases things like histamines and serotonin and kinins (proteins in the blood that cause inflammation, affect blood pressure and blood flow, stimulate pain receptors and allow fluids to more easily move through small blood vessels) that make our blood vessels dilate and let all our fluids out,” Pang explained. “The body starts to act like it’s really dehydrated, and the patient can get really unstable and die.”
An important step in successfully resuscitating a patient during that 24-hour burn shock period is to know the size of the burn. There are equations such as the modified Brooke formula used at TTUHSC, or classic equations such as the Parkland equation that tells a physician how much fluids a patient will require. The medical team can then titrate those fluids based on blood pressure, urine output and labs. However, the key to the entire process is correctly estimating the size of the burn.
Pang said that can be a problem, especially when burn treatment is sought from someone who may not handle burns frequently. And with Lubbock being the most rurally located burn unit in the nation, Pang and his colleagues see a significant number of patients transferring in for treatment from West Texas, New Mexico and the eastern Colorado areas. Because of the inexperience with burns in many of these areas, it’s very common for the referring facility’s TBSA estimate to be quite different from what Pang or other surgeons may eventually find.
“They may estimate the patient’s TBSA to be 27% burn based on what they know,” Pang said. “Then we get them and it may actually be 3% or 90%; it varies wildly, and as a result, these patients may get the wrong amount of fluid and do poorly.”
To help reduce the uncertainty inherent to TBSA measurements, the technology put forth by the Pang team focuses on two components: taking detailed photos and then accurately analyzing the photos to arrive at a more accurate TBSA result. The process includes removing the patient’s clothing to take a photo of their front, then rolling them over to take a picture of their back.
“With the algorithm or convolutional neural network that we've created, our hope is to be able to determine normal skin from burned skin and then calculate a number that tells us how big the burn is,” Pang said. “So far, we've had good luck with that. We still have some work to do, but we have a good foundation.”
The second component of the Pang team’s technology is to develop a prognostic or predictive quality to analyzing the photos. Pang said the team currently uses a traditional 80-20 training set where they take 80% of their images and plug them into the algorithm. The algorithm is then tested with the other 20% to see how well it does
“Right now, I believe our accuracy percentage is somewhere in the 80s,” Pang said. “Our goal is to get up into the 90s.”
Pang said the technology will help patients receive onsite care. If the EMT or other first responders don’t have burn experience, they can assess a burn accurately and relay that information to the burn providers earlier and more reliably. This also applies to outside emergency departments that don't have a burn center.
At the end of it all, Pang said the intent is to make the technology accessible via a cellular phone app so that an onsite EMT could strip someone who got burned, take two pictures, cover them back up and be able to communicate with burn physicians more effectively so care can be provided to patients almost immediately. This would lead to better outcomes such as preventing a burn from converting from a second-degree to a third-degree burn, which could save lives.
The technology also could lead to fewer and shorter hospital stays, less ICU days and reduced hospital costs. It could save patients time away from their normal life and help physicians practice with more confidence. Ultimately, Pang believes it could help people throughout every step of the process.
“We're just one of many people doing this kind of thing, but I think that health care and artificial intelligence, for the lack of a better term, is the future, and I think we're riding that wave,” Pang said. “I think you're going to see a lot of really cool stuff come out in the next six months to a year, and I think that health care is about to change, hopefully for the better, in an exponentially fast way. Honestly, I'm just happy to be here riding that wave.”
